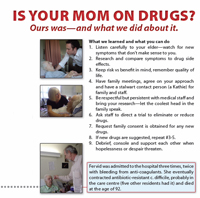
 Ours was. Here’s what we did about it
Ours was. Here’s what we did about it
Our Mom was occasionally a little forgetful — but cognitively with‐it and a leader in her retirement community. In 2003, at the age of 87, she was admitted to the Care Centre of her residence. The day before she’d asked her daughter to take her to the ER saying, “I knew I couldn’t stand without passing out.” She had been suffering from a bad cold but the ER found that although she did not have pneumonia, she was dehydrated with low sodium. She was given intravenous fluids and released. The next morning, still not feeling well, the nurse practitioner suggested a few days recuperation in the Health Centre and then a return to her apartment.
That’s how it all began. After admission to the care centre, instead of recuperating and returning to her apartment, her status declined precipitously. Two different SSRIs (antidepressants) had been tried without family consultation. The first one had given her hallucinations. Instead of depression, we saw her as mourning her loss: her apartment, independence, privacy and friends. Then she began experiencing severe mental status changes such as agitation, delusions, and inability to tell dreams from reality. She was “sleeping” and difficult to rouse even during the day — not a normal nap. She developed unexplainable, repetitive movements of her arm, sudden sweating, episodes of rapid heartbeat and lack of coordination. This was not our Mom!
Now on nine drugs, the staff said, “that’s not very many!” We suspected, after watching and listening carefully to what she said when lucid, that drug adverse effects could be the problem. I researched her drugs on reputable sources online, and I began to suspect her sudden deterioration was evidence of “serotonin syndrome” caused by drug interactions.
Meanwhile, we saw the plight of many residents and their isolation and loneliness, which has a huge impact on mental status. There is not a lot to remain sane for. Tiny ladies in wheelchairs approach you in the hallway and whisper, “help me, help me!” Long hallways resound with the noise of televisions from resident’s rooms while others sleep or stare blankly into space. Long stretches of isolation and doing nothing blur boundaries between sleeping, dreaming and waking. Interesting how apparent opposites can coexist to create the worst of both worlds: isolation and lack of privacy — anxiety and boredom.
Our family met first to coordinate our approach. Then, with research in hand, we met with medical staff, respectfully presented our research about drug interactions, with the goal of a directed “drug holiday” from the new drugs. We were successful. Meanwhile, the psychiatrist for the Centre had come through and prescribed donezipil for possible vascular dementia or Alzheimer’s. He said that a “scan” confirmed his diagnosis. He told us “her frontal lobe is shrinking.” My research on this revealed that everyone’s frontal lobe shrinks with age. We declined the drug he wanted to prescribe which had possible adverse effects and promised only a small, statistical benefit but no clinical effect. By this time, we had asked the medical staff not to prescribe anything we had not approved.
But listen to this — the “drug holiday” soon brought our Mom back cognitively! Completely!
Not only did her mental status return to normal, she improved physically — a contrast to her former bedridden and delusional state. She could participate in activities and exercise, attempting to circumvent her physiotherapist’s instructions and “training” new caregivers if she thought they needed it. She improved to the point that we would put her and the Centre’s fold‐up wheelchair in the car and drive to her favourite restaurant for oysters and white wine. This gave great joy to all of us. She had 3 years more of a good life though to our sorrow was never able to return to her residence — even to assisted living. She had been bedridden too long and lost enough function that she could not be discharged back to her residence. Losing 5% of functional muscle strength for every day in bed is standard for frail elders. Many who have been bedridden, either in acute or residential care, are then unable to return home.
Then, in November 2007, our Mom contracted antibiotic‐resistant clostridium difficile. Five other residents had it. It is a hospital‐acquired, antibiotic‐resistant “super‐bug.” She was not very sick with it but after several doses of a powerful antibiotic at each recurrence, she began to decline rapidly. Hydration was a problem and she also developed a stomach bleed because titration of her blood‐thinner was affected by diarrhea and not eating. Lack of appetite was compounded by the disgusting, ground‐up food she continued to receive because of previous swallowing difficulties that she no longer experienced. Have you ever seen a ground‐up grilled cheese sandwich — let alone eaten one?
Eventually Hospice Services were arranged in the summer of 2008 and she was taken off all drugs. Our Mom died in October 2008. She passed on her down‐to earth‐philosophy of life: “religion is about how you treat other people.” Her last weeks were remarkable and moving; she seemed intent on passing on what she’d learned about life and how much she loved us. We would never have received this gift if she had died several years earlier in a drug-induced, confused and delusional state.
To medical professionals:
Spending time with our Mom allowed us to observe, ask, and listen. We researched and compared her symptoms with adverse effects of drugs she was on. Doctors seldom do this. Symptoms are seen as another “condition” and more drugs ensue. This is known as the “prescribing cascade”. Our love and respect meant we left no stone unturned. Medical professionals don’t have time for that. They often don’t know their patient’s baseline of function and cognition, especially when first admitted to care. The family’s view is essential to keep patients safe and well. Seek it out instead of ignoring, disdaining, or even resenting it. Consider this also — could the so‐called Alzheimer’s and dementia “epidemic” be, in large part, a reflection of widespread and increasing over-medication of our elders?
To Canadians:
The media constantly decries unsustainable health care costs caused by aging “boomers” that will destroy Canada’s health care. I suggest this is an outcome only if we continue to practice medicine the way we do it now. Reduce over-medication of the elderly and we will reduce subsequent hospitalizations and need for residential care. This would result in huge savings. Most health care dollars are expended in people’s last few months of life. Most importantly, we could save a lot of suffering for our elders and their families. Lest you think I’m a crazed Pharma‐basher, and our experience an isolated incident, read A Bitter Pill: How the Medical System is Failing the Elderly (2009, Greystone Books) by Dr. John Sloan, a Vancouver GP who has worked almost exclusively with the frail elderly for a couple of decades. And if you want to read the over-medication bible, written by a consulting geriatric pharmacist, read: Are Your Prescriptions Killing You? by Armon Neel, Pharm D.
If you’re in your 70’s to 90’s, don’t make your kids repeat what we experienced. Talk to them and your family doctor; tell them how you want your life as an elder to go. Tell everyone about the dangers of over-medication of the frail elderly. Though research shows the negative physical and cognitive effects of polypharmacy on our elders, still it continues. If you’re over 60, you’re up next.
About the Contributor
Johanna Trimble is a respected family advocate based in Vancouver, BC. She is on the Steering Committee of Patient Voices Network of BC and a member of Patients for Patient Safety Canada, a working group of the Patient Safety Institute. She is a public member on two provincial continuing education initiatives for physicians: the Optimal Prescribing Update and Support Steering Committee and the Shared Care Polypharmacy Working Group. In October 2010, Johanna received a top award at an international medical conference in Amsterdam for her poster “Is Your Mom on Drugs?”.
